Note - we are publishing data for the weekend a day early because we plan to share a draft RFI response from Food Is Health with our readers on Friday morning for the “Ensuring Lawful Regulation and Unleashing Innovation To Make American Healthy Again”. If you have anything you think should be included, please send it to us TODAY. Think System C and the barriers - if you didn’t have a chance to read the background, please read this piece from last week.
Data for the Weekend
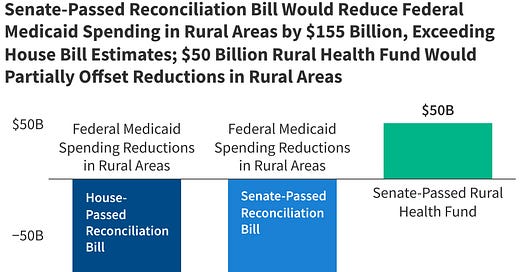
Now that the Big Beautiful Bill Act is law, the bulk of focus is on the impact it will have on rural healthcare, it seemed a fitting theme for this week’s data for the weekend.
“The impact on rural health and rural hospitals will be devastating”
- Aspen Health Strategy Group Meeting
We are interested in transforming Food and Health. To improve food, eliminate chronic disease, and remove the friction in longevity. Sooner or later, the healthcare system was going to break. Now is the time to transform.
Did You Know? Some Facts About Medicaid's Scope and Impact
To fix health, it helps to understand a bit of the scope of Medicaid, and the unique aspects of how the program funds care for chronic disease
23% of those losing Medicaid coverage under the Big Beautiful Bill Act reside in rural America (source)
Medicaid covers about 1 in 4 adults in rural America (in some states - AZ, NY, NM, LA and KY it is 1 in 3) - this accounts for half of all rural births and inpatient stays and covers 40% of children (in NM, LA and AZ it’s almost 60%). (source)
Medicaid reimbursement for vacciness is often less than the cost of the vaccines, forcing providers to either sustain losses to vaccinate patients or not vaccinate leading to further access barriers (source)
Medicaid covers 47% of all births in rural areas compared to 40% in metro areas. (source)
Medicaid patients are 21% less likely to die in a given year compared to uninsured patients (source)
Medicaid covers 23% of rural Americans under age 65 compared to 19% nationally (source)
Medicaid patients have 5 times higher odds of having at least one outpatient visit annually compared to uninsured (source)
75% of Medicaid-enrolled adults have one or more chronic conditions (source)
As of 10 years ago, residents of rural areas are almost 20% more likely to have 2-3 chronic conditions than their metropolitan peers (source)
Medicaid covers 16.1 million people in rural communities (source)
Rural hospitals could lose 21 cents of every dollar in Medicaid funding under proposed cuts (source)
Medicaid accounts for 10% of rural hospital net revenue ($12.2 billion nationally) (source)
In the past 10 years, 120 rural hospitals have either closed inpatient services or closed entirely (source)
Medicaid patients have 1.83 times higher odds of being diagnosed with hypertension compared to the uninsured. (source)
Medicaid patients have 1.69 times higher odds of having controlled hypertension compared to uninsured. (source)
40% of women of childbearing age in rural New Mexico and Louisiana are covered by Medicaid. (source)
Medicaid patients visit emergency rooms 2.86 times more frequently than non-Medicaid patients. (source)
Medicaid readmission rate for heart failure is 27.6 per 100 admissions vs 17.1 for private insurance. (source)
The Rural Health Fund meant to offset the cuts will be distributed as follows (source):
States will apply for funding
Funds could be used in a variety of ways, including promoting care interventions, paying for health care services, expanding the rural health workforce, and providing technical or operational assistance aimed at system transformation
50% of the funding equally distributed among states w/approved applications
50% allocated by CMS using a method that takes into account states’ rural populations w/in metro areas
Share of rural health facilities nationwide that are in a state
Situation of hospitals which serve a disproportionate number of low-income patients with special needs.
10 Ways Rural Healthcare Is Innovating Beyond Medicaid
Produce Prescription Programs are reversing chronic disease: Delta Produce RX in Mississippi provides low-income patients with $80 monthly credits for fresh produce at local grocery stores. Since 2020, participants have received nutritionist consultations and cooking classes alongside their "prescriptions," demonstrating how rural healthcare is treating food as medicine (source)
Mobile health clinics are delivering hospital-level care to remote areas: A digitally capable mobile health clinic in rural Minnesota provided 1,498 patient appointments by April 2022, offering telehealth consultations, laboratory testing, and primary care examinations to four underserved communities (source). Mobile clinics save the U.S. healthcare system over $1 billion annually in costs.
Direct Primary Care models are thriving where traditional healthcare fails: DPC practices eliminate insurance middlemen, providing predictable monthly fees that make healthcare accessible. Rural DPC clinics serve 25% of Health Professional Shortage Areas in rural locations, demonstrating that this model is effective where others are not.
Telepharmacy services are keeping communities connected to medication management: Rural pharmacies utilize telepharmacy models, where licensed pharmacists provide remote consultations to technicians, ensuring accurate prescriptions and effective patient counseling. Studies show no difference in medication quality between telepharmacies and traditional pharmacies.
Community Health Workers are bridging care gaps with local knowledge: The National Rural Health Association has trained over 500 rural CHWs who provide culturally competent care by leveraging their understanding of local communities. CHWs improve health outcomes and population health, especially for vulnerable populations.
340B drug savings are funding innovative rural services. Rural hospitals participating in 340B save $500,000 to $1 million annually, with 93% saying these savings help keep their doors open. They use funds for community health screenings, transportation services, and expanding rural health clinics to neighboring communities.
AI-powered mobile clinics are extending specialist capabilities. The University of Michigan leads a $25 million ARPA-H project developing AI systems that help general practitioners perform specialist-level procedures in mobile clinics. This technology enables physician assistants and nurses to handle complex procedures with real-time AI guidance.
Collaborative care models are achieving remarkable mental health outcomes. Rural clinics implementing collaborative care for depression enrolled 5,187 patients (15% of their adult population) and achieved significant improvements, with mean PHQ-9 scores dropping from 16.1 to 10.9. Three-quarters of participating clinics exceeded outcomes from controlled research trials.
Telehealth innovations are eliminating geographic barriers. Remote monitoring programs reduce emergency room door-to-physician time by 21 minutes and help avoid 700+ potential patient transfers. Rural providers use telehealth to provide specialty consultations, chronic disease management, and emergency response.
Rural FQHCs are expanding access through strategic growth. Despite organizational consolidation, rural FQHCs increased service delivery sites by 20% from 2017-2020, serving over 9 million patients across 5,356 locations.
These innovations show how rural America is innovating beyond medicaid alone. They represent opportunities to speed innovation through additional private investment and the dedicated focuse of entrepreneurs driving speed the transition to system C.
News
Starbucks Is Looking to Remove Canola Oil From Its Food Menu
Although there is yet to be official talk of the averge 40-65g of added sugars (which exceeds recommended daily sugar intake) in smaller Grande sized sweetened Starbucks drinks, Starbucks Corp. did announce they are exploring how to remove canola oil from its food lineup in the US and the company will add a new egg bite to its menu made with avocado oil
This comes on the heels of a meeting with RFK Jr to align with health priorities a few weeks ago
Social Posts
→ Food has changed: Through directed evolution and genetics, we have altered crops to boost yield, visual appeal, and sugar. Likely to the detriment of nutrients.
→ Evolution figured a lot out before we got in the way: Science seems to be a process of figuring out what evolution figured out a long time ago.
→ We could use a Steve Jobs, Sam Walton, or Bill Gates of “Food is Health”: If someone figures out how to eliminate the $1.9 trillion in healthcare cost from poor nutrition, is it Ok if they become a billionaire?
As social influencers continue to lead the path of “nutrition recommendations”, our friend
is co-hosting a webinar “Priorities to Improve Messages about the Healthfulness of Carbohydrate Food Sources for IAFNS - Advancing Food and Nutrition Sciences (link)Like it or not, AI is set to become deeply embedded in our day to day lives and interactions - it already is.
shared a recent experience on his holiday that really personifies the idea that we need to look less at whether AI belongs in clinical care delivery and more at the role of the doctor/clinician and think through what aspect should remain human and what aspect can be powered by AI. He used the term “passive hospitality” and shared the parallels with healthcare. Here is an exerpt…While co-founder of Superpower Max Marchione (who we interviewed recently for the podcast) stated he’s convinced we’ll see a new consumer health front door with AI rather than doctors. Again, mixing the word doctor interchangably with human.
Our friend Yuri Sudhakar at Nudj Health published a compelling and powerful case for Lifestyle Medicine through the Nudj Health program.
Meanwhile our friend
brought us back to the basics of soil reminding us that it’s not just about Medicaid cuts. He posted that 100 million acres of invasive grass is destroying our rangelands and cutting our carbon production. Further pointing out that 80% of grassland fires in Idaho in the past 10 years have been invasive dominated using Cheatgrass as the example of one that dries up before the natives and burns hotter and faster.















Curious to understand why food prescription programs generally seem to prioritize produce over more nutrient dense and satiating meat and dairy?