The recent changes to Medicaid are terrible.
The suffering for the 133 million Americans, nearly half the U.S. population, living with at least one chronic disease, is worse. And is expected to climb to 170 million by 2030. Add to the suffering the $400k-$450k in healthcare costs for those diagnosed with Type 2 diabetes.
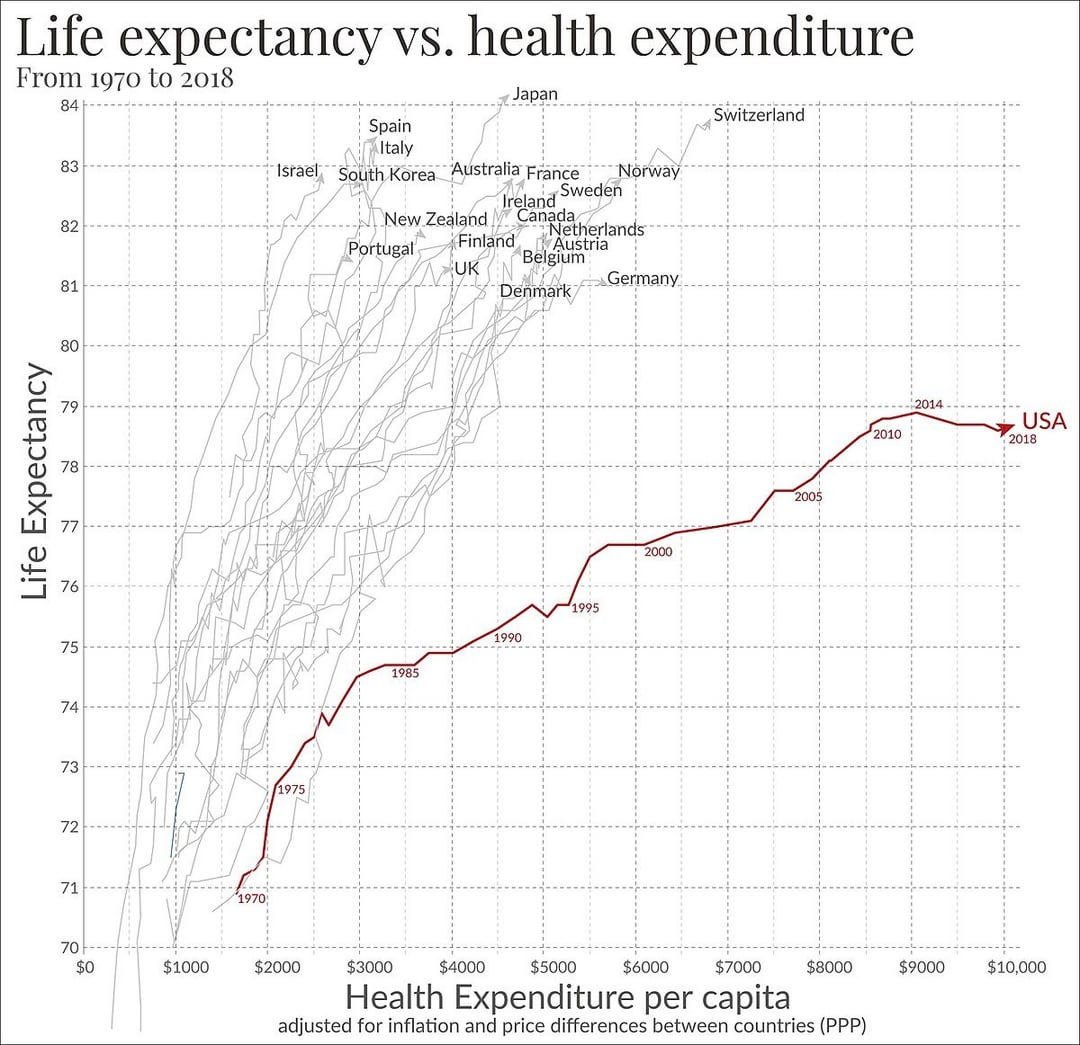
We have a system that pays more and more, fails to cure chronic disease, and increases its market size each year.
If we had no other choice, it would make sense for society to figure out a way to cover these healthcare costs. But we have other options. Difficult options, but not impossible.
We need to fix the food system.
Not all at once. Change is never all at once. Did you start using the internet in the late 60s when it was invented? Or in 2000, when it became mainstream. So it will be with food.
In the 1800s, we died of viruses and untreatable acute conditions. We invented vaccines, sanitation, antibiotics, etc. Our life span has increased. We then boosted the production of food. It weakened nutrition. And life span was cut short.
We were on a healthy track as recently as 1975. Chronic disease was not a significant issue for the preceding 350,000 years of human history. Our natural state is to be without chronic disease.
Frankly, it is easier to reform the food system than to twist our economy into financing an ever-increasing liability for chronic diseases.
Fixing food and health, however, is not a homogeneous affair. The economic dynamics in New York City are not the same as Bloomington Normal, IL. Rural health systems are likely to collapse in the near term. However, in its collapse, we may see the forces of agriculture, food, and healthcare reassemble to combat chronic disease and enhance healthcare. It is worse to think that we can return to a system of subsidizing a system that is out of control. We must press forward. Fix food. Fix health. End chronic disease. Build a healthcare system, better than anything anywhere, for everything but chronic disease. Because chronic disease will be a distant memory.
Rural Health
The combined Medicaid and Medicare cuts are likely the final straw for the current financial scheme keeping rural healthcare afloat.
On the surface, a 3-5% annual reduction in healthcare funding doesn’t seem dire. The problem is that the reduction is not spread evenly at all.
Healthcare in rural communities is dependent on an intricate web of the government (federal, state, and even local), cross-subsidization, an appropriate mix of business, grants, impact funding, private donors, and in some instances (e.g. Tenet & HCA) investors.
It’s akin to a Jenga puzzle. You pull the wrong piece, and everything tumbles down. For many rural healthcare systems, the cuts in “state-directed payments” will be that piece. Case in point, the reduction impact isn’t a blanket percentage, the following states are estimated to be hit hardest: MT 21%, AZ, KY and VA 18% each, CA 13% and NY 9%
In our current economic model for monetizing sickness, disease, and emergencies, there is no solution to keeping the doors open when the margin is reliant on reimbursement rates and patient volume. This is made worse when upwards of 20% of reimbursement is set to vanish for the most significant portion of the rural hospital patient population.
Traditional methods for winning at the Jenga puzzle are no longer viable options. The government gravy train is coming to an end, and employers and payers won’t bear the added cost of subsidizing this lost revenue.
As the uninsured population swells and the tsunami of uncompensated care hits, rural healthcare won’t know what to do. The government will be named the bad guy when, in fact, it’s our food industry and healthcare industry that placed us in this moment.
We are at a crossroads.
A New Path?
It’s time to finally forge the new path.
If we reverse chronic disease in the right amount and prevent it in the right amount of the pre-chronic population, the healthcare costs that would become uncompensated will vanish.
Some of the leading rural health systems continue to be stuck in monetization mode, deploying System C solutions of food and lifestyle medicine but doing so as community outreach and new revenue centers, service lines or bolt-on.
“We aren’t going back” sort of means burn the bridges behind you. It means a system redesign. It means tying the healthcare business model to outcomes, not CMS codes. It means care models that can finally reverse the disease at risk from funding cuts.
While these cuts will impact rural care systems, these communities may be the source of the solution. These are tightly woven communities with the ability to lead through a shared interest in agriculture, food, and health. These communities that run farm operations feeding the world, or on a whim, marshal resources for “Friday Night Lights”, are more than capable of rallying the community to improve food and health. Rural communities hold the skill to replace a healthcare economy built on disease with a food economy built on health.
But we can never go back to a system that monetizes chronic disease, fueling expense without solving the root cause. Our rural communities are a foundational element to the transformation of healthcare. They have the power to change food.
The Five Forces Toppling the Healthcare System
You've felt it in every doctor's waiting room. The sense that something fundamental is broken. Not just inefficient but backwards. A system that profits from your sickness and calls it healthcare.











Hi Ellen, Great article! I spoke to this recently here in terms of a systems approach: https://youtu.be/LirBzyqd31Y?si=OMNgu3C2y7L-YmuY